Value-Based Insurance Design Could Lower Healthcare Costs
As the cost of healthcare rises and the healthcare industry shifts from fee-for-service to value-based care, employers are also looking for ways to reduce costs without sacrificing care.
Value-based insurance design encourages healthy behaviors by offering employees incentives to use high-value services like chronic disease management and quality providers.
If you’re unfamiliar with the concept, here are five things to know about VBID according to the American Journal of Managed Care:
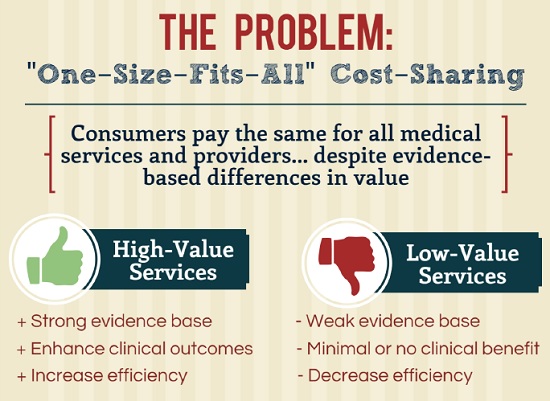
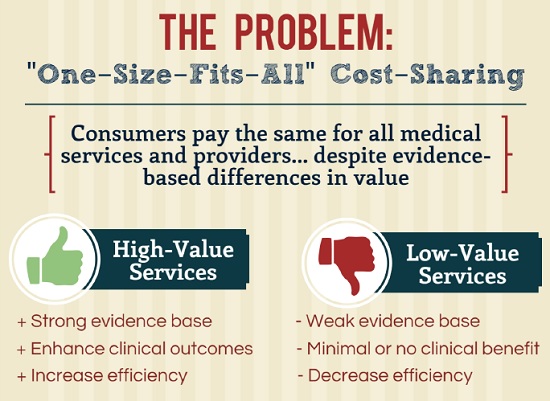
- Concept is 15 years old. The push for value-based care may just be gaining speed, but the concept of VBID was first introduced in 2001. The basic idea was that high-value services should cost less so they would be utilized more, and low-value services should cost more so they would be utilized less frequently.
- VBID uses clinical nuance. Clinical nuance recognizes that medical services differ in the benefit provided and that the benefit derived from a specific service can depend on the patient timing and location. Clinical nuance allows the healthcare industry to shift attention from how much we spend to how well we spend healthcare dollars.
- VBID plans can improve adherence. Studies support the notion that setting patients’ cost-sharing amounts in relation to the value the treatment offers can reduce barriers that prevent patients from receiving or taking treatments as prescribed.
- Employers are seeing benefits to implementing VBID. Employers are using VBID to encourage use of and increase access to evidence-based health services. Pitney Bowes created and launched a VBID initiative in 2002, making it the first company to fully implement this approach. Companies like Caterpillar, Hannaford Brothers Company, and UnitedHealthcare also use the VBID approach to improve employee health.
- Medicare Advantage pilot. Last year, the Centers for Medicare and Medicaid Services, announced that it would test whether providing Medicare Advantage organizations with the ability to integrate VBID would increase enrollee satisfaction, improve clinical outcomes, reduce plan expenditures, and save money. The model test is set to run five years in seven states: Arizona, Indiana, Iowa, Massachusetts, Oregon, Pennsylvania, and Tennessee.
RELATED
EXPLORE BY CATEGORY
Stay Connected with CBIA News Digests
The latest news and information delivered directly to your inbox.


