Paid Leave Authority Distributes $81M in Benefits

The Connecticut Paid Leave Authority distributed $81.2 million to 16,396 workers in the first six months of benefits availability.
The authority received 44,127 leave applications through the first six months of operation, approving 19,699 (60%) of the 32,701 decided claims while denying 13,002 (40%).
The undecided claims—26% of all applications—were either under review, awaiting final documentation, or were submitted well in advance of the target leave date.
Approved leave averaged 6.79 weeks according to the authority’s first annual report, with an average weekly benefit payment of $562.01.
Half of the received applications were for an employee’s own illness or injury, followed by bonding with a newborn (20%), pregnancy/childbirth (17%), and caring for a family member (12%).
Leave applications for family violence, adoption/foster care, organ donation, bone marrow donation, and military family leave made up the balance of claims.
Demographics
Claims by women represented 65% of all applications, while men filed 32% and those who identify as non-binary made up the balance.
The 26-41 age demographic filed more than half (53%) of all applications, followed by the 42-57 age group (24%) and 58-76 (17%).
Almost two-thirds (65%) of applications to care for a family member were submitted by women. Men represented 44% of child bonding applications.
“It is anticipated the usage rate will increase as public awareness of the program continues to build.”
Fairfield County, which has the largest population of the state’s eight counties, had the lowest number of claims per 10,000 residents (77.29).
New Haven County had the highest number of applications per 10,000 residents (140.37), with the City of New Haven responsible for 1,493 claims, the most of any municipality.
While total approved claims fell short of the six-month adjusted projection of 41,956, the authority’s report notes “it is anticipated the usage rate will increase as public awareness of the program continues to build.”
Denied Claims
Thirty-two percent of denied claims were COVID-related, with the authority approving just 7% of the 4,842 leave applications that were based on pandemic health conditions.
The report suggests that the “high denial rate on COVID cases skewed the overall denial rate upward.”
“The high denial rate on COVID cases skewed the overall denial rate upward.”
Failure to provide proper documentation was responsible for 77% of all denied claims, followed by non-qualified event (4%), claimant did not meet earnings requirement (3%), health condition not certified (3%), incomplete/insufficient information (3%), certification not received (3%), ineligible employee/employer (2%), and receiving other benefits (2%).
Individuals whose identity could not be verified, who did not work in Connecticut, who filed a claim outside the permissible window, and whose benefit entitlement was exhausted made up 3% of denied claims.
Program Benefits
Under legislation narrowly approved by the General Assembly in 2019, about 1.5 million Connecticut private sector employees must pay the 0.5% payroll tax that funds the program’s benefits and bureaucracy.
Most public sector workers are exempt from the tax—which the authority began collecting Jan. 1, 2021, with benefit payouts beginning Jan. 1, 2022.
Workers are eligible for up to 12 weeks of paid leave for a number of qualifying reasons, including a serious health condition of an employee or their family member, as well as a birth or adoption, among other life events.
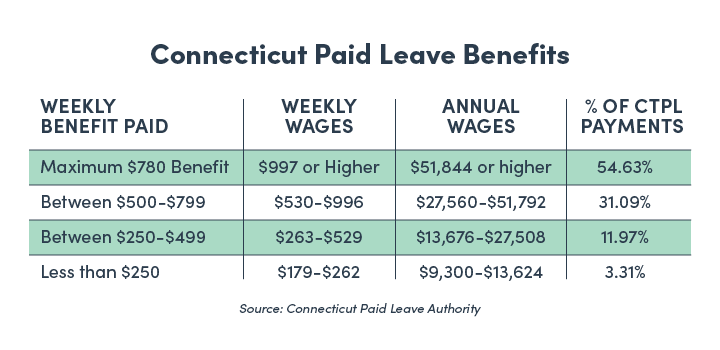
Program benefits are capped at 60 times the state’s hourly minimum wage—now $14 as of July 1, 2022—or $840 a week.
The maximum weekly benefit will increase to $900 when the minimum wage hits $15 next June.
The maximum weekly benefit will increase to $900 when the minimum wage hits $15 on June 1, 2023.
More than 137,000 businesses have registered with the authority—as mandated—with over $517.9 million in payroll taxes remitted to the paid leave fund, which has a balance of $390.9 million.
Businesses can use a private sector plan to comply with the state’s paid leave mandate. The authority has approved applications from 592 employers wanting to use a private sector plan.
The authority’s report shows employees tend to contribute less to private sector plans than the state collects, with those plans approving 82% of all claims.
RELATED
EXPLORE BY CATEGORY
Stay Connected with CBIA News Digests
The latest news and information delivered directly to your inbox.